Zika. Ebola. Influenza. Smallpox. The Plague. No matter how far back in human history you dare to look, you’ll find such scourges lurking alongside around, and inside the human body. Case by case, such diseases have lent themselves to our increased understanding of the science of us: how we get sick, how we get well again and ultimately, what happens when we don’t. By looking at all those cases as a whole, on an epidemiological or public health level, we began to learn even more about diseases and our vulnerability. Humanity began to understand how diseases are spread, and more vital perhaps, how to stop it from doing so.
There’s only one infectious disease we’ve managed to defeat. We’re still riding the high of having successfully eradicated smallpox—which ravaged humanity for millennia—just 37 years ago. A feat that was achieved through global surveillance and a nearly militant adherence to vaccination programs. Over the course of the last century, vaccines have given us a semblance of control over other potentially life-threatening infectious diseases, such as polio—the vaccine program for which was introduced in 1955.
Dr. Margaret Fearon, medical director of Medical Microbiology for the Canadian Blood Services in Toronto was a child when the polio vaccine was still fairly new. “I always remember my mother talking about how thankful everybody was, because every spring, parents of young children lived in fear that their child was going to get polio and either going to die, or end up in an iron lung.”
Over the course of her career, though, the attitude—you could even say gratitude—concerning vaccines has shifted. “The advent of the vaccine that would prevent [polio] was a miracle as far as they were concerned. But within one generation, we seem to have lost that. I think because parents these days never go through that fear of infectious diseases, for the most part, with their children.”
Parents of today who have not had to watch their child wither and die from smallpox or polio have vaccine protocols to thank for that. Of course, the present era is not free from fear: hysteria over the Zika outbreak in the last year, Ebola before that, and before that was severe acute respiratory system, or SARS, in 2003. Dr. Fearon remembers that outbreak quite well. Akin to the contagion-style horror flicks du jour, it started with a single person—a Patient Zero—and spread globally once he boarded an airplane.
“Any outbreak anywhere in the world is only a plane ride away,” Dr. Fearon says, “And I think we ignore that at our peril.” She points out that as the story of a major outbreak is unfolding, the media and perhaps even the government will pay attention—but that attentiveness doesn’t last. “It happens all the time in public health: you’re trying to persuade the funders that the money spent on preventive medicine, and on surveillance, is money that will save you big time down the road. Unfortunately, that lesson doesn’t persist very long after a large outbreak.”
The media’s focus isn’t always a particularly helpful one, either. Between the general population’s scanty health and science literacy and the news’ credo of “if it bleeds, it leads,” it’s not hard to see how the public can be easily led—or mislead—to panic. The problem is, that coverage—sensational or otherwise —occurs when the public health crisis has already arrived. Earlier, when its significance was increasingly pressing, it hadn’t yet become splashy enough to make headlines. And therein lies the problem.
Dr. Tara Smith, professor and leader of the Smith Emerging Infections Laboratory at Kent State University has devoted much of her decades-long career to antibiotic resistance. “I feel this is an area that maybe there’s not quite enough alarm in the general public,” Dr. Smith admits. While antibiotic resistance has certainly made headlines in the context of the sufficiently grisly Methicillin-resistant Staphylococcus aureus, or MRSA, it’s certainly not the only bacteria we have to worry about. And it may well not be the one we should be the most worried about. “We’re already there or very close to it for some infections,” Dr. Smith says, specifically noting multidrug-resistant tuberculosis and other “superbugs”; antimicrobial resistant infections. “As the population ages, we expect this to get even worse. But it’s much more like climate change: a slow burn rather than a sudden new outbreak, like Ebola or Zika. I think that makes it harder to raise awareness of it and explain the seriousness and potential magnitude of what losing antibiotics really means.”
It’s not just that pathogens are becoming resistant to the drugs we have, either. The problem is further compounded by the arduousness of creating new ones, “Antibiotic development is slow and, financially, a very risky move for pharmaceutical companies,” Dr. Smith points out, “The best thing you can do with a new antibiotic is use it sparingly for those who have untreatable infections, to minimize the chance of evolution of resistance—not a great financial model for a company needing to make a profit.”
It also doesn’t help that the major players who intersect in drug development—pharmaceuticals, government and clinical research—often tend to operate in silos. Without looking beyond the immediate task at hand, it’s easy to forget why antibiotics are so important in the first place. “In our global community, resistance anywhere can quickly become resistance everywhere,” Dr. Smith says, “So even if we were doing a great job controlling resistance in the U.S.—which we’re not—we’re still vulnerable due to what other countries are, or aren’t, doing.”
While we must remain vigilant in our quest to wrangle the diseases we know about, and which continue to evolve, we also have to take pains to ensure we aren’t making it any easier for them to do so (see: the anti-vaxxer movement and antibacterial hand soap). As befits the fictional arc of any outbreak movie, it may well be that as we’re creating or otherwise procuring the antidote to one threat, another is skulking around in the shadows in search of a suitable host.
Speaking of the chimerical coupling of science and story, it isn’t a stretch for virologist Dr. Anne Simon to imagine the far-reaching consequences of an unchecked, emerging virus for which humanity is woefully (and perhaps willfully) unprepared. In addition to being a professor at the University of Maryland, she’s been the science advisor on The X-Files, the eleventh season of which hits Fox this fall, since the show’s first season (fun fact: both she and Dr. Fearon got story credit on the final episode of the revival last year).
To conjure up a virus that can rise to the role of sine qua non plot device, Dr. Simon didn’t have to look too far beyond the facts. While the heroine of a science fiction flick might squint into a microscope and gasp as the fate of humanity comes into view, in reality, the power of a virus can’t be immediately ascertained at first sight. “For a lot of these emerging viruses, until they actually start infecting people—you don’t know,” Dr. Simon explains. “Things like Ebola are viruses that have more than just us as a host.”
Common vectors for disease—that is, what helps facilitate its spread—are critters like bats, rats and insects. It may be that the symbiosis between the two can go on for quite some time without any ill effect to the animal host or to any humans who encounter it. The trouble comes when the virus, at last, makes the leap from animals to us.
Avian influenza A (H7N9), several cases of which were reported to the WHO in China earlier this spring, is a present worry for many in the global public health sector. “Normally, these flu viruses are transmitted from pigs or birds to humans,” Dr. Simon says, “But they’re not transmitted human to human.”
It’s the cells the flu virus infects that determine its mode of transmission. In essence, it boils down to a “lock and key” type match between viral proteins and the surface of the cell itself. “If they infect cells in the lower respiratory tract, when you’re coughing, you don’t cough out the virus,” Dr. Simon notes, “It’s only when you have a flu virus that’s infecting cells in your upper respiratory tract that you cough the virus out, and then it gets transmitted person-to-person.”
The flu virus in China, while serious, doesn’t appear to have made that leap yet. The infected are primarily those handling poultry—although, two patients with lab-confirmed H7N9 reported to the WHO had no known poultry exposure, and the potential exposure of three other patients is still being investigated. Should it be determined that these cases were transmitted person-to-person, say, from one family member to another, that would change the game entirely.
While the dramatic, macabre nature of viral hemorrhagic fevers ( Ebola, Lassa, Marburg, etc) mean they’ll easily grab anyone’s attention should they appear in a headline or news ticker, influenza—while generally less bloody—is hardly trifling.
Historically, it’s proven to be one of the most lethal infectious diseases humanity has ever been up against.
Case and point: the H1N1 influenza pandemic of 1918. It’s estimated that a third of the world’s population was sickened, and it killed somewhere between 20-40 million people in a single year; more than the Black Death did in four. It struck people so severely and suddenly that they dropped dead in the streets. Physicians at the time, baffled by its aggressiveness, noted that their patients were literally suffocating to death from their own mucous with what they believed was “the most vicious type of pneumonia” they had ever seen.
One of the primary reasons it was so deadly was simply timing: people born in the previous century had been exposed to similar influenza strains in their lifetime and therefore enjoyed a limited degree of immunity. The younger generations were not so fortunate. In 2009, a novel strain of influenza A (H1N1) emerged and appeared to be a hybrid of several varieties of swine, bird, and human influenza viruses in North America and Europe. As with the flu in 1918, the young were hit particularly hard because they simply hadn’t lived long enough to be exposed to a variety of influenza strains.
That being said, influenza doesn’t have to be fancy-dancy to prove fatal. Despite the fact that it’s one of the more preventable causes of death, as we have an arsenal of vaccines for it which are constantly being refined, influenza kills about 250,000 to 500,000 people worldwide in a given year and causes severe illness in 3 to 5 million. The vast majority of the seriously ill being infants and children, pregnant women, the elderly, and those who are otherwise immunocompromised.
“People have a very relaxed attitude, when the reality is, if you look at the statistics, influenza has a huge impact on the population,” Dr. Fearon says, “Not just in one outbreak, but every winter with respect to morbidity and mortality.”
A global pandemic of the nouveau H1N1 was declared in the summer of 2009, just a few months after the new flu was identified. Thanks, at least in part, to a reasonable degree of pandemic preparedness it didn’t reach death tolls anywhere near that of the flu that struck us down at the turn of the century.
Yet despite our best efforts to get ahead, influenza keeps evolving. That’s why your previous year’s immunization may not prove effective for the next flu season, and thus, the vaccines are reworked annually. But there are also other viruses for which we’ve developed vaccines that have the potential to change the game on us via a phenomenon called “serotype replacement.”
As Dr. Smith explains, that’s when “the vaccine-included types become rarer due to herd immunity, but others that are not included in the vaccine become more common. This is a concern primarily with the HPV vaccine, with the pneumococcus vaccine, and with the Hib vaccine—as there are other types of Haemophilus influenzae that could replace serotype B. We’ve tried to get around that by adding serotypes to these vaccines to head this off at the pass, so to speak, but it’s a constant worry.”
This may also prove to be the epicenter of growing antibiotic resistance and vaccines, “We try to use vaccines to prevent some of these infections so we don’t need antibiotics to treat them—but what if the vaccines mean the proliferation of resistant strains not present in the vaccine?” Dr. Smith admits, “It’s a treadmill.”
The enduring frustration of trying to curtail infectious diseases like influenza is further beleaguered by the simple fact that they have multiple hosts. “If you think about smallpox and polio, they only had one host: us,” says Dr. Simon, “As soon as the last person had the virus—and everyone else kept away—there was no place for the virus to go, and that was the end of it.”
It’s not so simple when you consider viruses like Ebola, or even influenza, “If you want to get rid of the flu virus, you have a choice to kill every pig and bird the world. Then, I think, you could control it,” Dr. Simon supposes, “Or, you could not kill every bird in the world, and you know, let science try to control these viral infections and keep people as healthy as possible.”
A noble task for scientists, but one that’s pace is set not only by the inherent complexities of scientific inquiry but now, a hefty dose of sociopolitical encumbrance. And like, no pressure—but when it comes to getting the upper hand on whatever the next contagion will be, time is not necessarily a variable that’s on our side.
“The question is is not if, the question is when,” Dr. Simon states, “New viruses are emerging, and viruses that we already know about are changing.”
While odds are the next global pandemic won’t be the result of a nefarious government conspiracy involving extraterrestrials (though how’s that for a headline) it could be a pathogen that’s “alien” to us in the sense that it’s been hiding in the jungle for thousands of years, only to creep out now as the Earth warms. Or perhaps the churning and mingling of viral proteins will happily slither in through our dried-out, cracked, antibiotic-slathered hands. While outbreaks may feel sudden, and as though they came out of nowhere, that’s more a reflection of us than them. They are merely behaving in accordance with their nature in order to survive.
When we fail to heed the warnings and disease fells us, we have to ask ourselves: are we acting in accordance with ours?
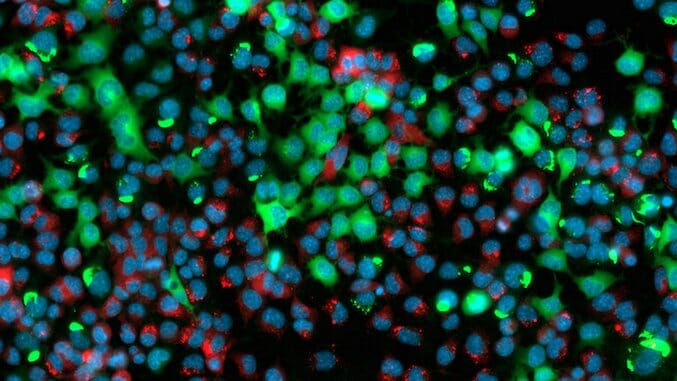
Photo by ZEISS Microscopy, CC BY 2.0
Abby Norman is a writer based in New England. Her first book, on medicine’s treatment of female pain, is forthcoming from Nation Books in March 2018. She’s a science editor at Futurism and the host of Let Me Google That on Anchor. Her work has been featured in The Rumpus, Atlas Obscura, The Establishment, Cosmopolitan, Seventeen, Medium, The Independent, and others. She’s represented by Tisse Takagi in New York City.