Stress Test: When Strain Becomes a Chronic Disease
Stress Test is a series about the science behind our busy lives and how stress affects our bodies. The biweekly column uncovers the latest research and explains how to put it to use in a practical way. Look for the science behind epigenetic markers of stress, mindfulness, meditation and deep brain stimulation.
![]()
More studies are linking stress to sickness, and some are making a direct connection to autoimmune diseases, or conditions that cause the immune system to attack healthy tissues. When the term “autoimmune disease” comes to mind, that often prompts thoughts about well-known conditions such as lupus, thyroid disease and rheumatoid arthritis.
A growing category of autoimmune diseases have caught media attention lately, especially as they relate to stress and lifestyle factors, including Celiac disease, Crohn’s disease, Hashimoto’s disease and irritable bowel syndrome.
Another category is burgeoning as well. Often hard to diagnose, these diseases seem to come from nowhere. They’re often classified as “idiopathic,” meaning they have no known cause and no known cure.
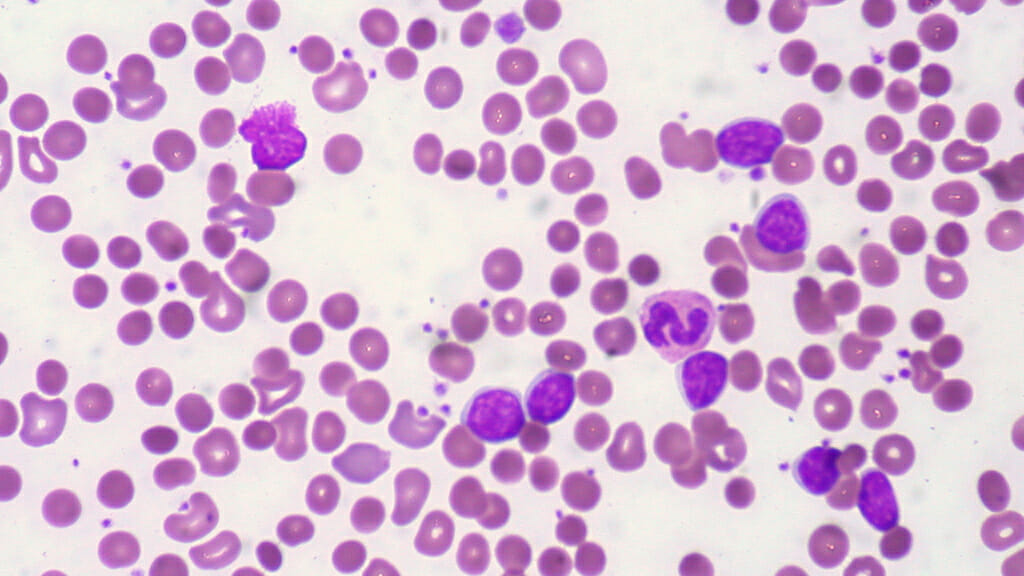
In fact, I was diagnosed with one of these stress-induced idiopathic diseases in 2010. After a year in a mind-blowingly stressful job, where I kept working even when I was sick in bed, I developed idiopathic thrombocytopenic purpura, an autoimmune disease that destroys the platelets in the blood. Essentially, if I got a cut, it would take a long time to clot. That’s nerve-wracking if you think about accidentally getting hurt — or even nicking yourself with a razor in the shower.
I left my stressful job and took a round of prednisone, and my symptoms have largely stayed at bay. But since then, I’ve met several people who mysteriously also have the same strange, unique disease. For my friends’ dad, for example, it meant he couldn’t fly for his job as a pilot until he got his platelet numbers back into the normal range. Scary stuff.
Here’s what scientists are reporting about the effects of stress on our immune systems:
1. Stress-induced autoimmune diseases are becoming more prevalent.
More than 50 million Americans live with an autoimmune disease, and 75 percent are women, according to the American Autoimmune Related Diseases Association. In fact, the Department of Health and Human Services’ Office of Women’s Health reports that autoimmune disease rank No. 1 in a top ten list of most popular health topics requested by callers at the National Womens’ Health Information Center (and womenshealth.gov).
Although the exact cause of autoimmune disease is multi-faceted — genetic, environmental, hormonal and immunological — researchers report that at least half are attributed to “unknown trigger factors.” Physical and psychological stress play a major part in that, scientists began emphasizing about a decade ago. They’ve also noted that a huge proportion – maybe up to 80 percent – of patients had uncommon emotional stress before an autoimmune disease occurred.
-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-

-